假性醛固酮减少症
外观
| 假性醛固酮减少症 | |
|---|---|
 | |
| Ⅰ型假性醛固酮减少症患者体内醛固酮含量增多(醛固酮增多症),但身体对其无法作出反应,症状与醛固酮减少症相似 | |
| 类型 | renal tubular transport disease[*] |
| 分类和外部资源 | |
| 醫學專科 | 腎臟科 |
| ICD-10 | N25.8 |
| eMedicine | 924100 |
| Orphanet | 444916 |
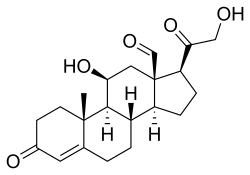
假性醛固酮减少症(pseudohypoaldosteronism,PHA),是一种症状类似醛固酮减少症的病症[1],系肇因于机体对醛固酮无法作出反应,负反馈调节抑制机制缺陷,导致醛固酮含量异常。
历史
[编辑]1958年,Cheek和Perry首次描述了此种综合征[2]。后来,儿科内分泌学家Aaron Hanukoglu称,假性醛固酮减少症有两种形态,遗传模式不同:一种是常染色体显性遗传的肾形态,主要表现为盐分自肾流失;另一种则是常染色体隐性遗传的多系统形态,表现为盐分自肾、肺、汗和唾液腺流失[3][4]。此二种统称Ⅰ型假性醛固酮减少症。
醛固酮反应异常的遗传缺陷至少有以下两种可能:1.与醛固酮结合的盐皮质激素受体突变,或2.醛固酮所调节的基因突变。对Ⅰ型假性醛固酮减少症患者进行的分析排除了第一种可能性[5]。后来,人们发现Ⅰ型假性醛固酮减少症是由基因SCNN1A、SCNN1B和SCNN1G突变导致的,这三个基因分别编码上皮钠通道亚基α、β和γ[6]。
类型
[编辑]| 类型 | OMIM | 基因 | 遗传 | 描述 |
|---|---|---|---|---|
| PHA1A | 177735 | MLR | 常染色体显性遗传 | 有钠流失 |
| PHA1B | 264350 | SCNN1A、SCNN1B、SCNN1G | 常染色体隐性遗传 | 有钠流失 |
| PHA2 | 145260 | WNK4、WNK1 | 无钠流失,可能与TRPV6有关[7] |
PHA2,即Ⅱ型假性醛固酮减少症,又名家族性高钾血症或戈登综合征,由Gordon于1986年首次描述,病因为潜在遗传缺陷导致肾脏远端小管氯化钠重吸收增加,进而导致体积膨胀、高血压、肾素水平降低。与Ⅰ型存在醛固酮抗性不同,Ⅱ型体积膨胀导致醛固酮水平降低。临床特征为高血压、高鉀血症、代谢性酸中毒,但肾功能正常[8]。
治疗
[编辑]Ⅰ型严重患者治疗需要较多氯化钠[9]。相反,Ⅱ型患者需要限制盐分,并使用噻嗪利尿剂阻断氯化钠重吸收,使血压、血钾水平恢复正常。
参考资料
[编辑]- ^ Pseudohypoaldosteronism: Overview - eMedicine Pediatrics: General Medicine. [2009-03-06]. (原始内容存档于2020-10-28).
- ^ Cheek, Donald B.; Perry, John W. A Salt Wasting Syndrome in Infancy. Archives of Disease in Childhood. 1958-06-01, 33 (169): 252-256. ISSN 0003-9888. PMC 2012226
 . PMID 13545877. doi:10.1136/adc.33.169.252 (英语).
. PMID 13545877. doi:10.1136/adc.33.169.252 (英语).
- ^ HANUKOGLU, AARON. Type I Pseudohypoaldosteronism Includes Two Clinically and Genetically Distinct Entities with either Renal or Multiple Target Organ Defects. The Journal of Clinical Endocrinology & Metabolism. 1991-11-01, 73 (5): 936-944. ISSN 0021-972X. PMID 1939532. doi:10.1210/jcem-73-5-936.
- ^ Hanukoglu, Israel; Hanukoglu, Aaron. Epithelial sodium channel (ENaC) family: Phylogeny, structure–function, tissue distribution, and associated inherited diseases. Gene. 2016-04-01, 579 (2): 95-132. ISSN 0378-1119. PMC 4756657
 . PMID 26772908. doi:10.1016/j.gene.2015.12.061.
. PMID 26772908. doi:10.1016/j.gene.2015.12.061.
- ^ Chung, E; Hanukoglu, A; Rees, M; Thompson, R; Dillon, M; Hanukoglu, I; Bistritzer, T; Kuhnle, U; Seckl, J; Gardiner, R M. Exclusion of the locus for autosomal recessive pseudohypoaldosteronism type 1 from the mineralocorticoid receptor gene region on human chromosome 4q by linkage analysis. The Journal of Clinical Endocrinology & Metabolism. 1995-11-01, 80 (11): 3341-3345. ISSN 0021-972X. PMID 7593448. doi:10.1210/jcem.80.11.7593448.
- ^ Chang, Sue S.; Grunder, Stefan; Hanukoglu, Aaron; Rösler, Ariel; Mathew, P. M.; Hanukoglu, Israel; Schild, Laurent; Lu, Yin; Shimkets, Richard A.; Nelson-Williams, Carol; Rossier, Bernard C. Mutations in subunits of the epithelial sodium channel cause salt wasting with hyperkalaemic acidosis, pseudohypoaldosteronism type 1. Nature Genetics. 1996-03, 12 (3): 248-253. ISSN 1546-1718. PMID 8589714. doi:10.1038/ng0396-248 (英语).
- ^ Yang, Sung-Sen; Hsu, Yu-Juei; Chiga, Motoko; Rai, Tatemitsu; Sasaki, Sei; Uchida, Shinichi; Lin, Shih-Hua. Mechanisms for Hypercalciuria in Pseudohypoaldosteronism Type II-Causing WNK4 Knock-In Mice. Endocrinology. 2010-04-01, 151 (4): 1829-1836. ISSN 0013-7227. PMID 20181799. doi:10.1210/en.2009-0951.
- ^ O’Shaughnessy, Kevin M. Gordon Syndrome: a continuing story. Pediatric Nephrology. 2015-11-01, 30 (11): 1903-1908. ISSN 1432-198X. PMID 25503323. doi:10.1007/s00467-014-2956-7 (英语).
- ^ Hanukoglu, Aaron; Hanukoglu, Israel. Clinical improvement in patients with autosomal recessive pseudohypoaldosteronism and the necessity for salt supplementation. Clinical and Experimental Nephrology. 2010-10-01, 14 (5): 518-519. ISSN 1437-7799. PMID 20661616. doi:10.1007/s10157-010-0326-8 (英语).
